The Problem
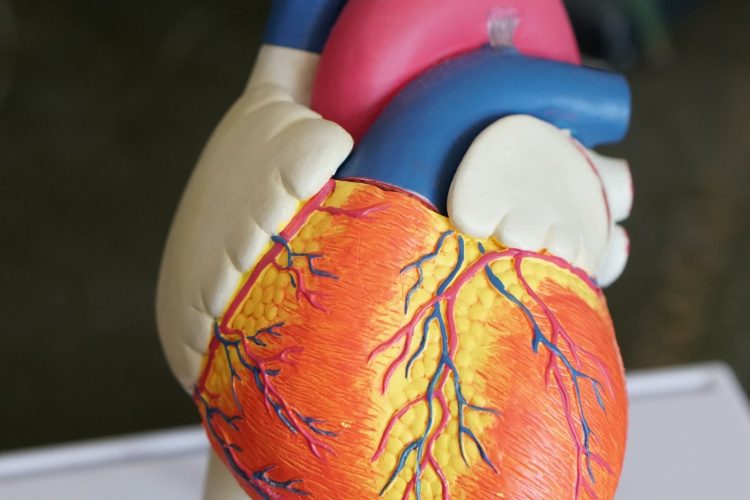
Cardiogenic shock is a state of cardiac dysfunction which leads to hypoperfusion of critical organs and can ultimately spiral into a fatal event. For the eight hundred patients who develop cardiogenic shock at Duke University Hospital (DUH) each year, their cohort’s in-hospital mortality rate of 30% represents a challenging set of patients who often require care coordination across multiple cardiac subspecialty teams.
Our Solution
Project goals:
- Develop a machine learning model to predict cardiac decompensation (v1: mortality)
- Use Duke EHR data (Epic + Lumedx) to generate and validate a digital cardiogenic shock phenotype
- Launch multi-disciplinary shock team
- Implementation goals: create visual dashboard of Aims 1 and 2 & validate both the model and phenotype
The Heart Center at Duke identified the opportunity to assess whether a new, expedited, team-based treatment intervention on these patients could improve the process of care and impact clinical outcomes. To support this new treatment intervention, Duke Cardiology and the Duke Institute for Health Innovation (DIHI) formed a transdisciplinary team to identify the patients who develop clinical deterioration and cardiogenic shock in real-time by creating an automated electronic phenotype, and to develop a machine-learning model for predicting in-hospital mortality for all Duke cardiac patients using patient baseline and hospital stay data extracted from the EHR. We will then combine the digital phenotype and model output in a visual tool to catalyze the deployment of the new team-based workflow and to help inform the clinical team’s treatment decisions.
We surveyed 230 Duke Cardiology clinicians on the potential value of a rapid intervention team and of a real-time mortality model output on patient care, and found that 80% of both physician and nurse sub-groups estimated a high or medium amount of value added by those care strategies for cardiology patient’s presenting early warning signs of deterioration. We designed a new multi-disciplinary cardiogenic shock team (Shock Team) workflow, which begins with the cardiac intensive care unit (CICU) fellow calling together the Shock Team after assessing a patient at risk for deterioration. The team consists of physicians in advanced heart failure, interventional cardiology, cardiac surgery, and the CICU. This team integrates the clinical tool (Shock Dashboard) that we developed into the care discussion to help risk stratify and determine the need for additional medical interventions, such as mechanical circulatory support.
Our team developed a four-part cardiogenic shock phenotype. The phenotype development cohort consisted of all adult DUH Cardiology patients over a 47-month timespan from October 2014 to August 2018, totaling 12,613 unique patients and 18,614 unique encounters. Our team used 377 clinically determined predictors including patient labs, vitals, and interventions to fit a lasso-penalized logistic regression, a ridge regression, a random forest, and an extreme gradient boosted decision tree model to predict inpatient mortality within a 48-hour window for DUH Cardiology patients at the time of admission into cardiology service (t0), and also at 4 hours (t4), 8 hours (t8), and 16 hours (t16) into the cardiology service admission (all maintaining the 48-hour window for mortality prediction). Inpatient mortality occurred in 180 (4.1%) of encounters. Models were developed on a subgroup of 2,721 patients (80%) and 3,543 encounters and models were evaluated on a held out, randomly-selected set of 680 patients (20%) and their 893 total associated encounters. We used cross-validation within the training set to tune model hyperparameters.
Impact
Resulting models for t0 had predictive performance area under receiver operator characteristic (AUROC) curve values ranging from 0.74 to 0.78 and area under precision recall (AUPR) curve values ranging from 0.06 to 0.09 calculated on the validation set. The t4, t8, and t16 models saw improved performance, ranging from 0.87 to 0.93 AUROC curve values, with AUPR curve values ranging from 0.20 to 0.36. Through additional analysis observations and discussion with cardiology leadership, we hypothesize that our performance improvement from the t0 model to the subsequent t4, t8, and t16 models largely due to the data available as the patient encounter evolves. We found that, for about half of our cohort, the time of admission into cardiology service (t0) corresponded to the time of admission into the hospital. Given that many of our model inputs involved lab results and procedures, we saw
Among our cohort of encounters, 4,767 (25.6%) met the phenotype. Within the phenotype, there are four definitions with specified criteria. Definition 1 specified concurrent reduced blood pressure and hypoperfusion indicators, as well as fever exclusion indicators during the encounter, with initial results showing that 1,867 of 18,614 cohort encounters (10.0%) met the definition. Phenotype definition 2 specified new or increased vasopressor administrations, with 2,160 of 18,614 encounters (11.6%) meeting this definition. Phenotype definition 3 involved identifying patients with a mechanical support device, with 2,088 of 18,614 encounters (11.2%) meeting this definition. Phenotype definition 4 involved identifying patients with worsening cardiac hemodynamics, with 1,246 of 18,614 unique encounters (6.7%) meeting criteria. The Shock Team was launched in April 2019, with 8 calls thus far to activate the team in response to a cardiac patient who seems to be deteriorating. Of those calls, two resulted in expedited surgeries (one VAD and one aortic valve surgery), one resulted in stabilization for advanced heart failure therapies, and one resulted in treatment with medications and PCI.