At many institutions across the country, the barrier has been thick and stone-like between the Academic Health Center and the faculty and staff at the University. Duke has been taking the necessary steps to tear down this barrier with new care models as the pickax. In order to create better, more personalized, care for patients, healthcare institutions like Duke Health must be able to analyze data in real time to understand the risks of individual patients and tailor care according to that risk. In partnership between the Duke Institute for Health Innovation (DIHI), the Department of Statistics, and the Department of Bioinformatics and Biostatistics, Duke has begun to develop tools that harness machine learning to understand the risks of surgical complications and rate of chronic kidney disease decompensation to tailor care for individual patients.
DIHI is currently supporting two innovation project teams that bring together these domains of expertise. Professor Katherine Heller and three PhD students (Stephanie Brown, Elizabeth Lorenzi, and Joseph Futoma), in the Department of Statistics, serve as machine learning experts for both projects. Mark Sendak, a data scientist at DIHI, along with a new team of statistics and computer science interns (Joshua Taylor, Ouwen Huang, Kelvin Niu, Alice Ni, and Michael Gao), serve as data scientists for both projects. Finally, surgeons (Drs. Jeff Sun, Erich Huang, Christopher Mantyh, and Julie Thacker), and nephrologists (Drs. Blake Cameron and Uptal Patel) serve as clinical experts.
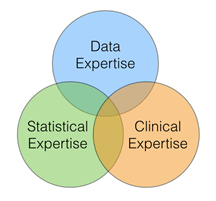
To effectively integrate machine learning into change within the clinical workflow, three sets of expertise must converge: data expertise, statistical expertise, and clinical expertise. The emergence of data science enables analysis of local data that has been unprecedented. Instead of working with well-curated, highly organized clinical trial data, data scientists excel at wading through and exploring structured and unstructured data collected as a product of care delivery. Thus, opportunities and paths towards improving care emerge that statisticians and clinicians collaborate to address.
But we have found that the areas of distinct expertise are less valuable than the areas of overlap that enable effective communication and collaboration. Three of the physicians are programmers or informaticians, the lead data scientist is a medical student and two interns are pre-med, and the lead statistics faculty has training in neuroscience.
The promise of a medical center to leverage the wealth of multi-disciplinary talent to learn from health data and transform the organization through these learnings exists at Duke. For more information or to submit an idea for collaboration with the experts, please contact us here.