An Overview
Sepsis is a clinical condition that is common, dangerous, and expensive. Nationally, patients diagnosed with sepsis have a 28% mortality rate, and sepsis constitutes the single greatest cost to Medicare for inpatient hospitalizations. Early detection and treatment of sepsis is key to improving clinical outcomes. However, sepsis is poorly understood at a pathophysiologic level, and as a result, the condition is difficult for clinicians to diagnose and treat effectively. At the Duke Institute for Health Innovation, we developed and implemented a deep learning model into clinical care to provide an early warning system within Duke Health for patients who are at risk of sepsis. In addition to the deep learning model, we have developed a software infrastructure that includes:
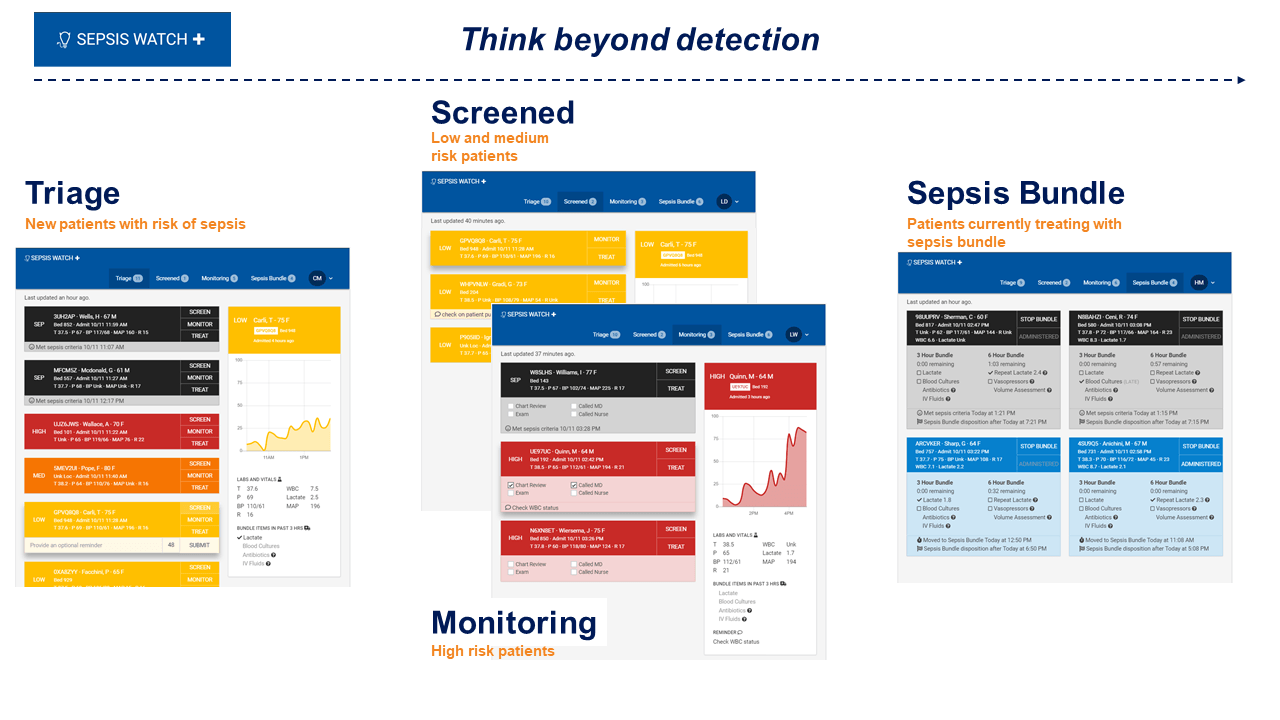
- EHR data cleaning and processing code
- A pre-launch model optimization, workflow, and evaluation planning tool
- A dashboard user interface to display information on high-risk patients, facilitate the clinical workflow, and monitor the delivery of sepsis treatment bundle elements
- A quality improvement tool to track key performance and utilization metrics in real-time and facilitate continuous improvement
Since going live with Sepsis Watch™ in November 2018, Duke has doubled its 3-hour SEP-1 bundle compliance, as reported each quarter to the Center for Medicare and Medicaid Services.
The Opportunity
The widespread adoption of electronic health records (EHRs) has enabled health systems to harness insights derived from clinical data like never before. With new availability of health data, clinical decision support tools based on predictive analytics have become popular means by which to improve diagnostic accuracy. At the Duke Institute for Health Innovation, we worked with Dr. Cara O’Brien and her team to understand how we could leverage our EHR to identify patients at risk of sepsis before they might present clinically. Within a year and a half, we worked with our local technology solutions team and statistical partners to pull retrospective health data and develop a sepsis prediction model that outperforms traditional clinical risk scores and other standard machine learning techniques. Our analysis showed that our early warning system could predict sepsis a median time of 5 hours before clinical presentation and, given the high morbidity and mortality of sepsis, had the potential to save 8 lives a month. However, the question still remained: how do you develop an analytics-driven clinical workflow to bring the full potential of such a technology to realization? Our approach was three-pronged: 1) evaluate our prediction model for its ability to provide clinicians with prospective and actionable insights, 2) engage key stakeholders in our effector arm to ensure seamless integration of this technology with clinical practice, and 3) build capacity and infrastructure across Duke Health to promote sustainable growth in the field of predictive health analytics.
Deriving Actionable Insights
Data-driven insights are useless unless they provide relevant and actionable information to clinicians. A prediction engine that warns of deterioration 72 hours in advance for a patient who looks completely healthy creates confusion in care delivery and raises a medical and ethical conundrum. To avoid such a predicament, we trained our model to predict sepsis within a more actionable time window of 12 hours to drive clinical decisions for all patients captured by our early warning system.
End-to-End Integration with Clinical Practice
After refinement of our model, we needed to ensure that we constructed a proper workflow to rapidly triage, reassess, and treat sepsis for all patients in our pilot site. We estimated caseload across different sites in the hospital and ultimately decided to partner with the Emergency Department (ED) as our initial site for deployment. We trained a centralized team of Rapid Response Team (RRT) nurses, with previous experience in managing clinical deterioration, to evaluate model output on a custom-developed risk stratification tool. Lastly, we worked with key stakeholders in Duke Health leadership, RRT, and the ED to develop the touchpoints between clinician and machine and establish a protocol for elevating clinical concern for at-risk patients.
Building Capacity for the Future
Our sepsis program will be one of Duke Health’s first clinical workflows to leverage machine learning to prospectively identify and treat disease. To facilitate an environment in which superior analytic techniques are regularly incorporated to inform clinical practice, we as a health system must develop capacity in infrastructure and people. Our team has been working with clinical and technical leaders to develop the governance and monitoring of such analytics-driven clinical workflows. Only through a better understanding of the strengths and limitations of such analytic approaches, thoughtful integration into clinical practice, and a clear strategy for monitoring and maintaining these systems can we develop a novel health system framework to leverage these technologies to improve our patient care.